“Delivering on the quality and shared savings promises.”
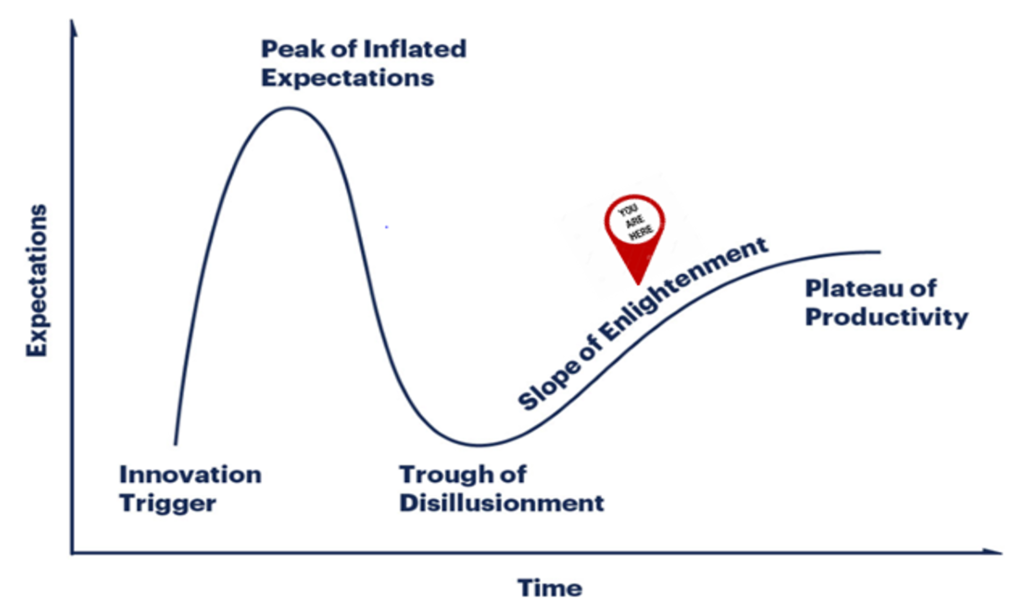
In the previous post, we discussed the Provider-Owned ISNPs journey through Gartner’s Hype Cycle and identified a key indicator of Provider-Owned ISNPs transition from Slope of Enlightenment to the Plateau of Productivity as: “Criteria for assessing provider viability are more clearly defined”
For Provider-Owned ISNPs, this viability criteria includes: experience, clinical integration, and well-capitalized scale.
Gartner’s Hype Cycle
Operating a nursing home is hard. American Health Plan’s sister company American Health Communities experiences this daily across our 29 SNFs. However, the complexity of operating a Medicare Advantage (MA) Plan brings unique challenges. These plans sit in the pivot of data and flow of funds between members, providers, and CMS. Navigating through the data and flow of funds without experience is challenging.
The Medicare Advantage industry is dominated by large operators like Humana and United Healthcare. The industry is also relatively young. Medicare Advantage only became policy in 2004. Very few executive teams have founded, developed, grown and operated Medicare Advantage plans at scale. American Health Plans has this experience, and the learnings that come with it. While experience does not eliminate all challenges, it helps our nursing home partners avoid expensive missteps and to navigate new challenges more confidentially.
Integrated and Comprehensive
ISNPs are a coordinated dance between execution of the Model of Care, facility engagement, enrollment activities and plan operation initiatives like network development. Ironically, the most common fragmentation we see in poorly operated ISNPs occurs with the dance lead: Execution of the Model of Care. Properly executed Model of Care ensures coordination of care management and clinical support, with the goal of proactively addressing the medical needs of each resident to prevent unnecessary hospitalizations. A care management team consists of a nurse practitioner or physician assistant, a nurse manager, a pharmacist, and other members staff who are available 24 hours a day / 7 days a week.
As such, American Health Plans takes a comprehensive approach to ISNP management, inclusive of the Model of Care through our care management entity, TruHealth. Starting an ISNP without a proven, integrated care management program is like building a house without the mortar. The building will go up quickly, but you’ll soon be back-tracking to fill in the gaps and keep the structure together
Well-capitalized for Scale
Medicare Advantage Plans require capital. An operating partner that doesn’t put up the majority of the capital ends up being a vendor rather than a partner. This leads to issues when more operating resources are required. In our model, American Health Plans puts up at least half of the capital in our joint ventures. This means we are accountable, and our partners know we are prioritizing the health of the plan. In addition, we syndicate out the provider ownership component, which allows for smaller nursing home organizations to participate.
This approach to ISNP execution allows smaller nursing operators with scale to access this opportunity. We give them access to capital not ordinarily available, and they bring additional scale to the joint venture.
It took some time, and some early adopters hard experience, but the Provider-Owned ISNP playbook is clear. Nursing home operators can benefit from full risk arrangements by leveraging a partners’ experience and capital in a clinically integrated operating model.
We welcome your feedback, so comment below or reach out directly at HWatson@AmHealthPlans.com